A periapical abscess is a collection of pus that occurs at the root tip as a result of bacterial infection. The periapical abscess usually occurs when bacteria spread to the tooth pulp through a crack or dental caries. It can cause tooth pain, swelling, and other symptoms. The pain increases in severity over a few hours or days, and when you put pressure or heat on the affected tooth. Also, the pain can sometimes radiate to other areas such as the ear, jaw, neck. If you suspect that you have a periapical abscess, visit your dentist as soon as possible for treatment. Your dentist will drain the pus, relieve the pain, and eliminate the infection. If a periapical abscess is left untreated, it can lead to serious, even life-threatening complications. In this article, we will discuss:
- What causes a periapical abscess?
- What are the signs and symptoms?
- How a periapical abscess is treated?
- Can a periapical abscess go away on its own?
- How do you know if a tooth abscess has spread?
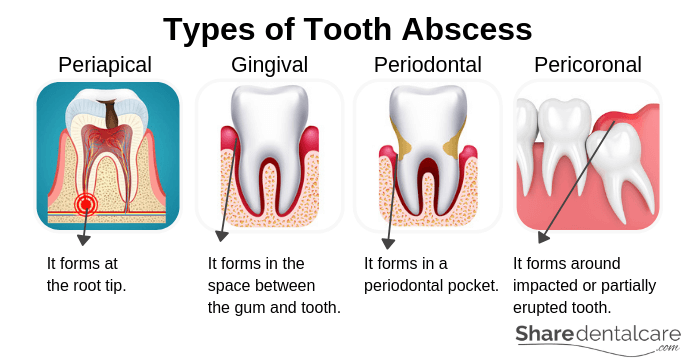
Types of Tooth Abscess
There are several types of tooth abscess. A periapical abscess is one of them. Each type occurs in a different area for a different reason. The types of tooth abscess include:
- Periapical abscess: it is the most common type. A periapical abscess occurs at the root tip as a result of untreated dental caries, crack, or trauma. Bacteria invade the pulp through dental caries or crack in the tooth, causing inflammation of the pulp tissues and the formation of the abscess at the root tip.
- Gingival abscess: this type usually occurs when foreign-body or food is trapped in the space between the tooth and the gum near the coronal part of the gum. To treat the gingival abscess, your dentist will remove the trapped foreign-body or food and clean the area with saline (salt water).
- Periodontal abscess: this type is associated with gum disease and begins in an infected periodontal pocket. In contrast to a periapical abscess, the tooth associated with a periodontal abscess is usually vital. To treat the abscess, your dentist will clean the infected periodontal pocket and perform scaling and root
planing to prevent the recurrence of infection. Note: periodontal pockets occur due to the destruction of tooth-supporting tissues and bone as a result of advanced gum disease (periodontitis). - Pericoronal abscess: it usually occurs within the gum tissue covering a partially erupted or impacted tooth. The
pericoronal abscess is usually associated with impacted or partially erupted lower wisdom tooth. The treatment includes the removal of gum tissue covering the wisdom tooth or the extraction of the wisdom tooth.
Symptoms of Periapical Abscess
Periapical abscess causes persistent, throbbing toothache that increases in severity over the following hours or days. Also, the pain can radiate to the ear, jaw, or neck. Other signs and symptoms include:
- Persistent, growing, sharp, throbbing pain in the affected tooth and surrounding gum.
- The pain may radiate to the ear, jaw, and neck.
- Hot foods and drinks cause pain.
- Biting or chewing on the affected tooth cause pain.
- The pain gets worse when you lie down.
- Swelling and redness of the gum surrounding the affected tooth.
- Pus pocket in the gums.
- Swelling and redness in the face.
- Discoloration of the affected tooth.
- The affected tooth becomes loose.
- Bad breath and a foul taste in the mouth.
- The lymph nodes under your jaw become tender and swollen.
- Difficulty breathing or swallowing.
Pain Management
The periapical abscess usually causes pain that increases in severity over the following hours or days. Over-the-counter (OTC) pain relievers may help you control the pain until you are able to see your dentist. For example, ibuprofen, paracetamol, and aspirin. Read more about warnings and precautions before using OTC pain relievers. Also, consult your doctor or pharmacist if you have/are:
- Medical conditions such as asthma, stomach bleeding, history of stomach problems, high blood pressure, liver disease, or kidney disease.
- Pregnant or breastfeeding.
- Allergic reaction from taking pain relievers.
- Taking other medications that may interfere with pain relievers.
Home remedies to Reduce the Pain
While you are waiting to see your dentist, you can try these home remedies to reduce the pain:
- Avoid hot or cold foods and drinks. Changes in the temperature may cause extreme pain.
- Avoid eating acidic or sugary foods.
- Don’t chew on the affected side and avoid hard foods.
- Eat cool, soft foods if possible.
- Keep your head elevated during sleep. Because the blood rushes to your head when you lie down, causing extreme pain that keeps you awake.
- Don’t floss around the affected tooth and use a soft-bristled toothbrush.
- Use over-the-counter pain relievers such as ibuprofen and paracetamol.
Causes of Periapical Abscess
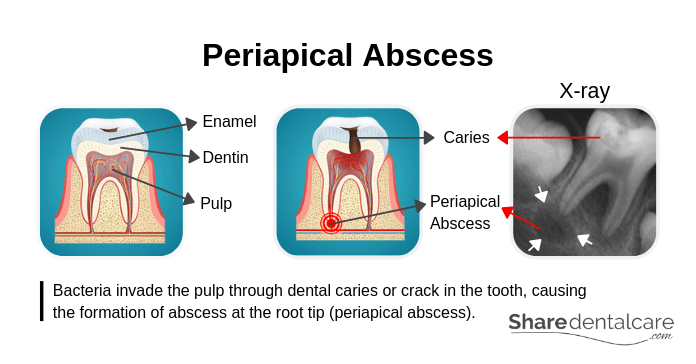
Each tooth consists of enamel, dentin, and pulp. The enamel is the outer layer of the tooth and the hardest substance in the human body. Also, it covers the dentin which is the second layer in the tooth. Both enamel and dentin protect the pulp which contains sensitive nerve tissues and blood vessels. Bacteria invade the pulp through dental caries or crack in the tooth, causing the inflammation of the pulp, persistent toothache, and the formation of abscess at the root tip (periapical abscess). On x-ray, the periapical abscess appears as a dark area surrounding the root tip.
Risk Factors
A periapical abscess occurs as a result of untreated dental caries or crack in the tooth. There are several factors that may increase your risk of a periapical abscess, include:
- Inadequate oral hygiene: not brushing your teeth regularly and flossing can increase the risk of dental caries and tooth abscess.
- Consumption of sugary foods and drinks: such as sweets and sodas. Also, foods that stick to your teeth for a long time such as dried fruits and cookies can increase the risk of dental caries.
- Dry mouth: saliva washes away your teeth and counteracts the acid produced by bacteria which help prevent dental caries. Dry mouth occurs often due to certain health conditions, certain medications, drinking alcohol, or smoking.
- Broken tooth filling: it can lead to the accumulation of food debris and plaque more easily, causing the formation of dental caries.
- Teeth grinding: physical injury, chewing hard foods such as ice or candy, and grinding your teeth can lead to the development of cracks in teeth.
- Medical conditions: heartburn and gastroesophageal reflux disease (GERD) can cause wear of the tooth enamel, exposing the dentin. This can lead to the development of dental caries more easily.
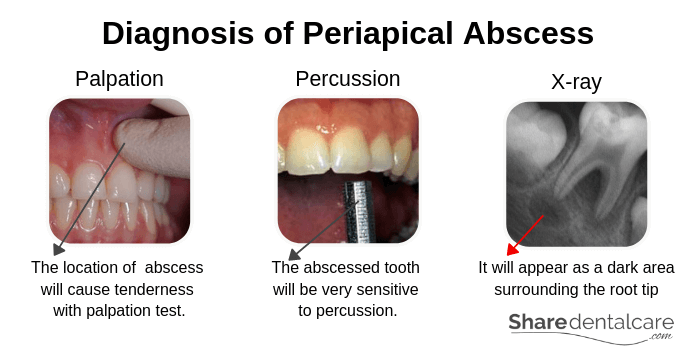
Diagnosis of Periapical abscess
Your dentist will examine the affected tooth and surrounding gums. Sometimes, it is difficult to distinguish between periodontal and periapical abscess. So, your dentist will perform a clinical examination and take an x-ray.
- Palpation: it is an important part of the clinical examination. Your dentist will use one hand to determine the location of the periapical abscess. The location of tooth abscess will cause tenderness with palpation test.
- Percussion test: in the clinical examination, your dentist will use an instrument to tap on the affected tooth. The abscessed tooth will cause pain with pressure or tapping (percussion).
- X-rays: your dentist will take an x-ray to identify the location tooth abscess. The periapical abscess causes changes in the bony tissue surrounding the root tip. It will appear as a dark area surrounding the root tip on x-ray.
- CT scan: your dentist may ask for a CT scan if he/she suspects that the infection has spread to other parts of the body such as the neck.
Treatment of Periapical Abscess
If you suspect that you have a periapical abscess, you should visit your dentist as soon as possible. Because periapical abscess won’t go away on its own and untreated abscess may spread to other areas such as the jaw and neck. Also, periapical abscess can’t be treated at home. So, visit your dentist as soon as possible to relieve the pain and eliminate the infection. The treatment includes:
- Drainage of the abscess: in the case of a large periapical abscess, your dentist may drain the abscess through a small cut (incision) in the gum. Then, he/she will clean the area with saline. Abscess drainage is a temporary solution to relieve the pain and speed the healing, and you will need further treatment.
- Root canal treatment: it involves cleaning of the root canals with instruments (dental files) and disinfectant solution to remove inflamed or dead pulp tissues and eliminate the infection. Then, the dentist will fill the root canals with a material called gutta percha and restore the tooth crown with tooth fillings such as amalgam or composite.
- Tooth extraction: in the case of a severely damaged tooth, you may need to extract the affected tooth to eliminate the infection.
- Scaling and root
planing : sometimes, the periapical abscess occurs due to the spread of bacterial infection from periodontal pockets to the dental pulp. It is known as Perio-Endo lesions. The treatment includes root canal treatment followed by scaling and root planing.
Periapical Abscess Antibiotics
Your dentist will prescribe antibiotics if the periapical abscess is severe or has already spread to other parts of the body such as the neck to help bring the infection under control. Tell your dentist if you have a medical condition, an allergic reaction to certain antibiotics or taking other medications that may interfere with the prescribed antibiotics. Antibiotics are only there to bring the dental infection under control and can’t replace the dental treatment.
When to See a Dentist?
If you suspect that you have a periapical abscess, visit your dentist as soon as possible. Also, contact your dentist immediately if the periapical abscess is associated with facial swelling or fever. Go to the emergency room if you have these signs and symptoms:
- High temperature (fever) more than 38°C.
- Severe facial swelling.
- Severe pain can’t be reduced by OTC pain relievers.
- Difficulty opening your mouth, swallowing, or breathing.
- Swelling of the neck, under the jaw, or around the eye.
- Tenderness of the lymph nodes in the neck.
These are the signs and symptoms of a serious infection that requires immediate treatment.
Complications of Periapical Abscess
An untreated periapical abscess can spread to other parts of the body, causing serious, even life-threatening complications. For example:
- Periapical cyst: it is a pathological cavity that develops around the root tip because of the death of pulp tissues.
- Maxillary sinusitis: the infection may spread to the maxillary sinus, causing inflammation of the maxillary sinus, headache, foul-smelling nasal discharge, and fever.
- Ludwig’s angina: it is a potentially life-threatening condition that occurs when the infection spread to the floor of the mouth, underneath the tongue.
- Osteomyelitis: it is a bone infection that occurs due to the spread of periapical abscess bacteria through the bloodstream into the bone.
- Sepsis: it is a potentially life-threatening condition that occurs when the body’s response to infection causes injuries and damage to multiple organ systems.
Prevention of Periapical Abscess
A periapical abscess is a complication of dental caries. To prevent tooth abscess and caries, you should:
- Brush your teeth and floss regularly: brush your teeth at least twice a day with a soft-bristled toothbrush and use fluoride toothpaste. Also, use dental floss to clean the spaces between your teeth that can’t be reached by a toothbrush.
- Eat healthy food: eat a balanced diet that contains a variety of different foods. Also, limit sugary or acidic foods and drinks, and between meal snacks.
- Visit your dentist regularly: visit your dentist at least once every 6 months for professional teeth cleaning and regular oral examinations to prevent dental caries and treat them early.
Conclusion
Do you have persistent, throbbing tooth pain? Do you suspect that you have a periapical abscess? You should visit your dentist as soon as possible. Because periapical abscess won’t go away on its own and untreated tooth abscess may spread to other areas, causing serious, even life-threatening complications. Over-the-counter (OTC) pain relievers can help you control the pain until you are able to see your dentist. Also, avoid hot or cold foods and drinks, don’t chew on the affected tooth, and sleep with your head elevated. At the dental office, your dentist will identify the underlying cause, reduce the pain, and treat the problem.