A periodontal abscess is a collection of pus that occurs in the tooth-supporting tissues (the periodontium) as a result of bacterial infection. It usually occurs as a complication of advanced gum disease (periodontitis), which is caused by poor oral hygiene. The periodontal abscess causes pain that becomes worse with biting on the affected tooth. Also, the pain may spread to the ear, jaw, and neck. Other signs and symptoms include gum redness, swelling, pus discharge, and bad breath. Visit your dentist as soon as possible if you have the symptoms of a periodontal abscess. An untreated tooth abscess can cause serious, even life-threatening complications. In this article, we will discuss:
- What are the signs and symptoms?
- What causes a periodontal abscess?
- Can a periodontal abscess go away without treatment?
- What happens if the abscess is left untreated?
- How to treat a periodontal abscess?
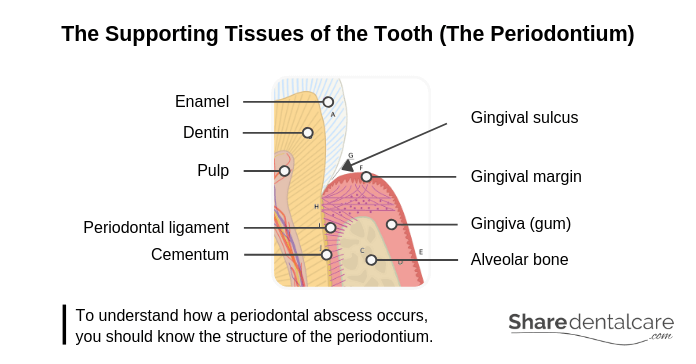
What is The Periodontium?
The periodontium is the specialized tissues that hold the tooth in its place and support the tooth during its function. To understand how a periodontal abscess occurs, you should know the structure of the periodontium, which includes:
- Gingiva (gum): it is the mucosal tissue that covers the mandible and maxilla, and surrounds the teeth. Usually, the color of healthy gingiva ranges from light coral pink to darker pink with melanin pigmentation. In the case of inflammation, the gingiva becomes red and swollen with an increased tendency to bleed.
- Periodontal ligament (PDL): it is a group of connective tissue fibers that attach teeth to the surrounding alveolar bone. It is attached to the alveolar bone from one side and the tooth root (cementum) from the other side.
- Cementum: it is a bone-like tissue that covers the surface of tooth roots. The cementum provides the attachment of the tooth to the alveolar bone by anchoring the periodontal ligament (PDL).
- Alveolar bone: it is a part of the upper and lower jaws that holds the teeth and support them during their functions.
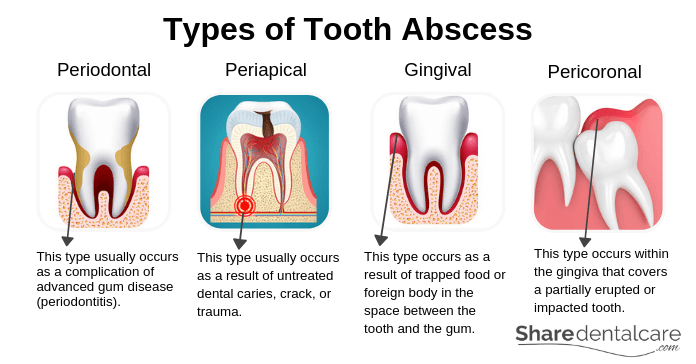
Types of Tooth Abscess
The periodontal abscess is a type of tooth abscess. The other types are periapical, gingival, and pericoronal abscess. Each type of tooth abscess occurs in a different location for a different cause.
Periodontal Abscess
A periodontal abscess usually occurs as a complication of advanced gum disease (periodontitis). Poor oral hygiene can lead to the inflammation of the gum tissues surrounding the teeth (gingivitis). The gums become red and bleed easily during tooth brushing. The inflammation may worsen over time (periodontitis), causing the destruction of the periodontal ligament, the loss of bone that supports teeth, and the formation of periodontal pockets (deep space around teeth). If these pockets become infected, this will lead to the formation of a periodontal abscess. Sometimes, the periodontal abscess occurs due to the spread of the infection from the pulp within a tooth (periapical abscess) through the periodontal ligament. This is known as combined Endo-Perio lesion.
Periapical Abscess
A periapical abscess usually occurs as a result of untreated dental caries, crack, or trauma. Bacteria can spread to the pulp within a tooth through dental caries or crack, leading to the death of pulp tissues and formation of a periapical abscess. Sometimes, the periapical abscess can occur due to the spread of infection from a periodontal pocket to the tooth pulp via accessory canals. This is known as combined Perio-Endo Lesion.
Gingival Abscess
A gingival abscess occurs as a result of trapped food or foreign body in the space between the tooth and the gum near the coronal part of the gum. Gingival abscess doesn’t affect the periodontal ligament that supports the tooth.
Pericoronal Abscess
A pericoronal abscess occurs within the gingiva that covers a partially erupted or impacted tooth. Poor oral hygiene can lead to the accumulation of bacteria around the gum tissue that covers a partially erupted or impacted tooth, causing inflammation (pericoronitis). If this inflammation is left untreated, it may cause pain and the formation of an abscess (pericoronal abscess).
Symptoms of Periodontal Abscess
The periodontal abscess causes pain that gets worse when you bite on the affected tooth. Other signs and symptoms of the periodontal abscess include:
- Sudden, throbbing, persistent pain.
- Redness of the gum.
- The gum is swollen and painful to touch.
- Pain with biting or chewing.
- Tooth mobility.
- A pocket of pus in the gums.
- Bad taste due to pus discharge.
- Bad breath.
- The pain may radiate to the jaw, ear, and neck.
- Fever and fatigue.
- Tenderness and swelling of the lymph nodes under your jaw.
- Difficulty swallowing and breathing.
Pain Management
The periodontal abscess usually causes pain that gets worse when you bite or chew on the affected tooth. You may need over-the-counter (OTC) painkillers to control the pain until you can see your dentist. OTC painkillers include ibuprofen, paracetamol, and aspirin. You need to consult your dentist or pharmacist before using OTC painkillers, especially if you:
- Are pregnant or breastfeeding.
- Have asthma, stomach bleeding, blood pressure, liver disease, kidney disease, or other medical conditions.
- Have an allergic reaction to a certain type of painkillers.
- Taking other medications that may interfere with painkillers.
Home Remedies to Control The Pain
Periodontal abscess can’t be treated at home. However, you can try these home remedies to control the pain until you can see your dentist:
- Rinse your mouth with warm salt-water.
- Avoid biting or chewing on the affected tooth.
- Eat on the opposite side of your mouth.
- Eat soft foods if possible.
- Maintain good oral hygiene and use a soft-bristled toothbrush.
- Use OTC painkillers such as ibuprofen, paracetamol, and aspirin.
These home remedies may help you control the pain temporarily. However, you shouldn’t use them to delay your visit to the dentist.
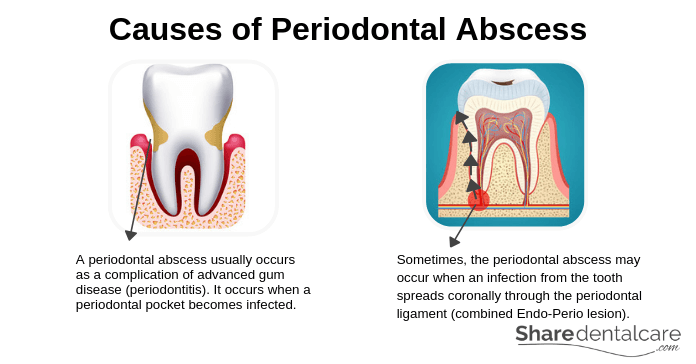
Causes of Periodontal Abscess
A periodontal abscess usually occurs as a complication of advanced gum disease (periodontitis). With inadequate oral hygiene, bacteria and food debris accumulate on your gums, causing the inflammation of gums and gum bleeding. This is the early stage of gum disease which is known as gingivitis. When gingivitis is left untreated, the inflammation may spread to the tooth-supporting tissues (the periodontium), causing periodontitis which is an advanced form of gum disease. Periodontitis can lead to the destruction of the periodontal ligament, alveolar bone loss, and formation of periodontal pockets between your gums and teeth. These pockets can become infected, causing pain and the formation of a periodontal abscess.
Sometimes, the periodontal abscess may occur secondary to a periapical abscess. This condition is known as combined Endo-Perio lesion. Bacteria enter the tooth pulp through dental caries or crack, causing the death of the pulp and formation of a periapical abscess at the root tip. Then, the infection may spread coronally through the periodontal ligament (PDL), causing a periodontal abscess.
Risk Factors
A periodontal abscess occurs as a complication of periodontitis (advanced gum disease). Several factors may increase the risk of tooth abscess, include:
- Poor oral hygiene: plaque is the primary cause of gum disease. So, not brushing or flossing your teeth daily can lead to the development of periodontitis and periodontal abscess.
- Smoking and tobacco use: smoking is linked to serious medical conditions such as lung disease and cancer. Also, smoking and tobacco use increase the risk of periodontitis.
- Teeth grinding: clenching or grinding your teeth puts an excessive force on the periodontium (teeth-supporting tissues), leading to the destruction of these tissues and the formation of periodontal pockets.
- Dry mouth: having a dry mouth can increase your risk of gum disease and dental caries. Dry mouth often occurs as a side effect of some medications or due to medical conditions.
- Poor nutrition: Poor nutrition can compromise your body’s immune system and make it difficult for your body to fight infection which increases the risk of periodontitis and periodontal abscess.
- Medications: some medications can affect the health of your gums, such as antidepressants, oral contraceptives, and certain heart medications.
- Medical conditions: some medical conditions can worsen the condition of your gums, such as diabetes mellitus, cardiovascular disease, and rheumatoid arthritis.
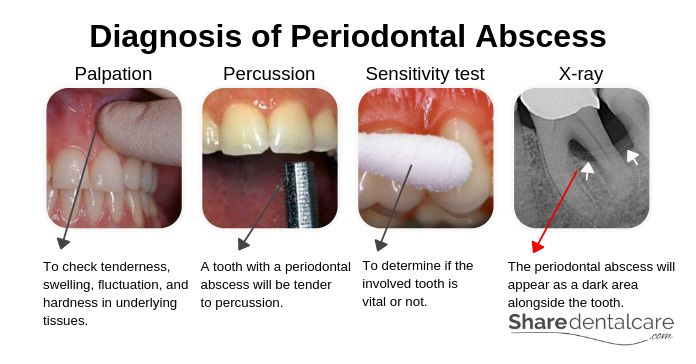
Diagnosis of Periodontal Disease
Visit your dentist as soon as possible if you have persistent pain, swelling, bad taste, or pain with chewing or biting. Your dentist will examine your oral cavity with a dental mirror and probe to identify the cause of these signs and symptoms. Sometimes, it is difficult to differentiate between periodontal and periapical abscess. So, your dentist will perform some examinations such as:
- Palpation test: your dentist will examine your oral cavity (intraoral examination) with his/her index finger to check tenderness, swelling, fluctuation, and hardness in underlying tissues. Also, your dentist will examine the lymph nodes (extraoral examination) to check if the infection has spread.
- Percussion test: your dentist will tap on your teeth with the end of a mirror handle. A tooth with a periodontal abscess will be more tender to horizontal percussion (perpendicular to the long axis of the tooth). A tooth with a periapical abscess will be more tender to vertical percussion (with the long axis of the tooth).
- Sensitivity tests: they are performed to determine if the involved tooth is vital or not. The periodontal abscess is usually associated with a vital tooth while the periapical abscess is associated with a non-vital tooth.
- X-ray: the periapical abscess will appear as a dark area (radiolucent) surrounding the root tip on an x-ray while the periodontal abscess will appear as a dark area alongside the tooth due to the destruction of PDL and bone loss.
- CT scan: your dentist may order a computed tomography (CT) scan to check if the infection has spread to other areas such as the neck.
Treatment of Periodontal Abscess
Periodontal abscess won’t go away on its own and should be treated in the dental office. An untreated tooth abscess may spread to other parts of the body, for example, jaw and neck. So, visit your dentist as soon as possible to treat the infection and relieve the pain. The treatment includes:
- Drainage of the abscess: in a large periodontal abscess, your dentist may drain the abscess to relieve the pain and control the infection. However, this is a temporary solution and you will need further treatment.
- Scaling and root planing: it is also known as non-surgical periodontal therapy. Your dentist may perform scaling and root planing to clean the periodontal pockets, and remove dental plaque and calculus. This will help in the treatment of periodontal disease and speed the healing of the periodontium.
- Tooth extraction: if the tooth-supporting tissues (the periodontium) are severely destructed with tooth mobility, or there is a history of a recurrent abscess, or the tooth prognosis is poor, your dentist will extract the involved tooth.
- Root canal treatment: periodontal abscess is usually associated with a vital tooth. However, it may occur due to the death of pulp tissues and the spread of infection to the bone surrounding the root tip then coronally through the periodontal ligament. In this case, your dentist will perform a root canal treatment followed by scaling and root planing.
Periodontal Abscess Antibiotics
If the periodontal abscess is severe or has already spread to other areas, for example, jaw and neck, your dentist will prescribe antibiotics to bring the infection under control and prevent complications. Then, you will need further treatment such as scaling and root planing, root canal treatment, or tooth extraction. Before taking antibiotics, you should tell your dentist if you:
- Are pregnant or breastfeeding.
- Have an allergic reaction to certain medications.
- Taking other medications.
- Have medical conditions such as kidney disease, liver disease, or a history of stomach problems.
When to See a Dentist?
Visit your dentist as soon as possible if you have persistent pain, gum swelling, pus discharge, or pain that gets worse with biting. Go to the emergency room (ER) if the periodontal abscess is associated with:
- Fever (more than 38°C).
- Severe facial swelling.
- Severe pain that can’t be controlled by OTC painkillers.
- Tenderness or swelling of the lymph nodes in your neck.
- Difficulty breathing or swallowing.
These signs and symptoms indicate that the infection has spread to other parts of the body and require immediate treatment.
Complications of Periodontal Abscess
Periodontal abscess won’t go away on its own. It needs to be treated as soon as possible. An untreated periodontal abscess can spread to other parts of the body, leading to serious, even life-threatening complications.
- Maxillary sinusitis: the infection may spread to the spaces that are located below the cheeks, above the teeth on the sides of the nose. These spaces are known as maxillary sinuses.
- Ludwig’s angina: rarely, the infection may spread to the floor of the mouth underneath the tongue, causing swelling around the mandible, difficulty swallowing, neck pain, swelling of the neck, and difficulty breathing. Ludwig’s angina is a life-threatening condition.
- Sepsis: rarely, the infection may travel to the bloodstream, causing a life-threatening complication known as sepsis.
- Osteomyelitis: the infection can travel through the bloodstream into the bone, causing pain, swelling, and fever. This condition is known as osteomyelitis. It is a rare but serious condition. Osteomyelitis usually affects the bone near the site of infection. However, the infection can travel through the bloodstream and affect any bone in the body.
Prevention of Periodontal Abscess
A periodontal abscess usually occurs as a complication of advanced gum disease (periodontitis). So, keep your gums and teeth healthy to prevent tooth abscess. You should:
- Practice good oral hygiene: brush and floss your teeth regularly to remove food debris and plaque trapped between your teeth and gums. Also, use fluoride toothpaste and mouthwash to help prevent or reduce gingivitis.
- Quit smoking: smoking is one of the biggest risk factors in the development of gum disease. According to the Centers for Disease Control and Prevention (CDC), smoking weakens your immune system, making it harder to fight a gum infection and also making it harder for your gum to heal.
- Regular professional cleaning: your dentist can detect the early signs and symptoms of gum disease. So, you should visit your dentist at least once every 6 months to remove tartar (calculus) and treat gingivitis before it becomes more serious.
Conclusion
Do you have throbbing, persistent pain and gum swelling? Does the pain get worse when you chew or bite? First, you have to visit your dentist as soon as possible to identify the underlying cause, relieve the pain, and eliminate the infection. You can’t treat a periodontal abscess at home. If the abscess is left untreated, it may spread to other areas such as the neck causing serious complications. Until you can see your dentist, use OTC painkillers to control the pain and don’t chew on the affected area.