A dental implant procedure is a surgical procedure that involves the placement of artificial tooth roots (similar in shape to screws) into the jawbone to replace missing teeth. These artificial tooth roots provide support for dental prostheses (crowns, bridges, or dentures). A conventional dental implant consists of 3 parts: the implant body, abutment, and dental prosthesis. The implant body is made of titanium or zirconia, which are compatible with the human body. The dentist or oral surgeon places the implant body surgically into the jawbone, underneath the gum. Then, the bone grows and fuses with the implant body (osseointegration). The osseointegration can take several months (4 to 6 months), depending on the quality of the bone. After that, the dentist or oral surgeon attaches the abutment and dental prosthesis to the implant body. In this article, we will discuss:
- Parts of a dental implant.
- Are you a good candidate for the dental implant procedure?
- How long does the procedure?
- Dental implant procedure step by step.
- What is bone grafting?
- Post-operative instructions.
- Risks and complications.
Parts of a Dental Implant
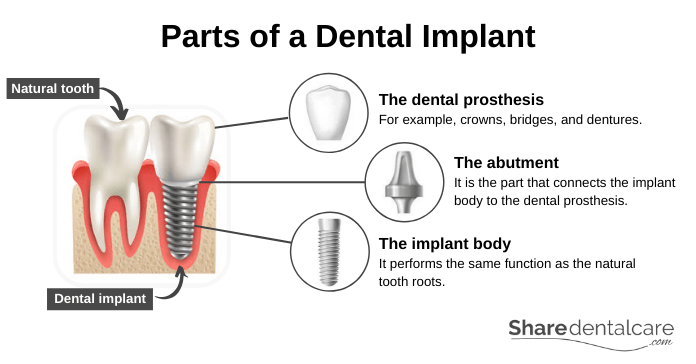
To understand how a dental implant procedure is performed, you should know the parts of the dental implant. A conventional dental implant consists of 3 parts: the implant body, abutment, and dental prosthesis.
- The implant body: it is similar in shape to screws and performs the same function as the natural tooth roots. The dentist or oral surgeon places the implant body surgically into the jawbone, underneath the gum. The implant body is made of titanium or zirconia, which are compatible with the human body. So, the bone fuses with the implant body. This process is known as osseointegration, which can take from 4 to 6 months.
- The abutment: it is the part that connects the implant body to the dental prosthesis (crown, bridge, or denture). The dentist or oral surgeon attaches the abutment and dental prosthesis after the healing period (4 to 6 months).
- The dental prosthesis: for example, crowns, bridges, and dentures. The selection of dental prostheses depends on several factors, such as the number of missing teeth, quality of bone, economic factors, and patient preference.
Are You a Good Candidate for the Dental Implant Procedure?
If you have one or more missing teeth, you are a good candidate for dental implant procedure if you:
- Have a healthy bone and healthy gums.
- Have enough bone length and thickness.
- You can undergo oral surgery.
- Don’t have a medical condition that may affect bone healing.
- Don’t smoke.
- Have good oral hygiene.
You can talk to your dentist to see if the dental implant procedure is the right option for you.
Contraindications
The dental implant procedure is suitable for almost all patients. However, it is contraindicated in the following cases:
- In children and adolescents.
- During pregnancy.
- Maxillary sinus or nerves are too close to the implant.
- Severe bruxism.
- Heavy smokers.
- Alcohol abuse or drug abuse.
- Patients undergoing radiotherapy.
- Patients with medical conditions such as:
- Poorly controlled diabetes mellitus.
- Kidney or liver disease.
- Acute infectious disease
- Immunological diseases.
- Osteoporosis.
- Active cancer.
Diabetes mellitus and smoking increase the risk of dental implant procedure failure. However, they won’t prevent the procedure. Each patient needs to be evaluated on an individual basis. So, visit your dentist to discuss with him/her the right treatment option for you.
How Long Does a Dental Implant Procedure Take?
Placing a dental implant in the jawbone takes around an hour. However, the entire dental implant procedure takes 6 to 8 months. Bone grafting will increase the total time of the procedure.
Dental Implant Procedure Timeline
- Initial Consultation: During the first visit, your dentist will examine your mouth, take a dental impression, and ask for a cone-beam computed tomography (CBCT) to evaluate the quality and quantity of the jawbone.
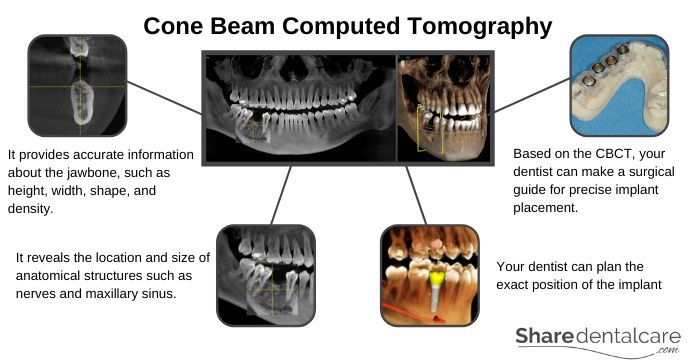
- In-depth assessment: on the next visit, your dentist will use the CBCT to check the height, width, and density of the jawbone, and plan the exact position of the implant. Based on the CBCT, your dentist can make a surgical guide for precise implant placement (surgical stent). Then, your dentist will schedule an appointment for dental implant surgery.
- Bone grafting: if the jawbone is insufficient, your dentist may recommend a bone grafting procedure, which will take an additional 3 to 4 months to heal.
- Placement surgery: on the day of the surgery your dentist will take around an hour to place the implant in the jawbone.
- Healing period: your dentist will leave the implant to fuse with the surrounding bone (osseointegration) for 4 to 6 months, depending on the density of bone.
- Attachment of the prosthesis: This is the final step in the dental implant procedure. After the osseointegration is complete, your dentist will attach the abutment to the implant body and then take a dental impression for the fabrication of the dental prosthesis (crown, bridge, or denture). At last, your dentist will attach the dental prosthesis to the abutment.
Dental Implant Procedure Step-by-Step
Pre-Operative Planning
A successful dental implant procedure depends on detailed pre-operative planning and preparation. Before the procedure, your dentist will:
Review your medical history
Your dentist will review your dental history, social habits, and medical history. If you are a smoker, your dentist will strongly advise you to stop smoking before the dental implant procedure. Because smoking makes your mouth drier, which can promote the growth of bacteria and worsen the condition of your gums. Also, the nicotine reduces the blood flow, which affects the healing process and immune response, causing implant failure. Tell your dentist about previous or existing medical conditions you have and medications you take to avoid any unnecessary complications. Medical conditions such as diabetes mellitus, cancer, radiotherapy, and alcoholism can affect the healing process, causing implant failure.
Examine your oral cavity
Your dentist will examine your oral cavity, take a dental impression, and take x-rays to evaluate the missing teeth area and determine how many implants you need. Also, your dentist will ask for a cone-beam computed tomography (CBCT) to determine the quality and quantity of the jawbone. The CBCT provides accurate information about the jawbone, such as height, width, shape, and density. Also, the CBCT reveals the proximity, location, and size of anatomical structures such as nerves and maxillary sinus. Based on the CBCT, your dentist can plan the exact position of the implant and make a surgical guide for precise implant placement (surgical stent).
Make the treatment plan
To make a treatment plan, your dentist will use your x-rays, CBCT, and study model. The treatment plan depends on several factors, such as the number of missing teeth, the proximity of anatomical structures, the type of dental prosthesis, and the quality and density of the jawbone. As a part of pre-operative planning, your dentist will treat existing dental problems such as dental caries and gum disease.
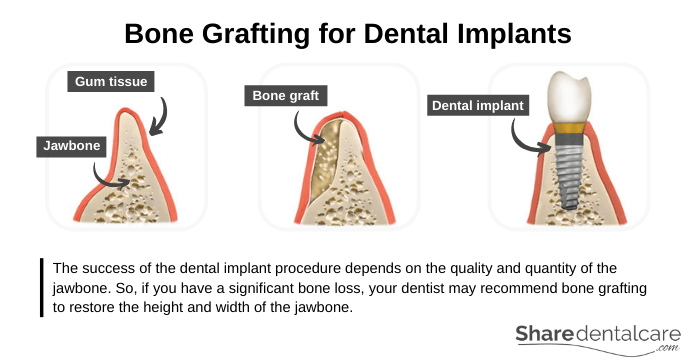
Bone Grafting
The success of the dental implant procedure depends on the quality and quantity of the jawbone. If your jawbone is too thin, soft, or insufficient, the implants could fail over time. So, you may need a bone graft to create a more solid base for the implants. Bone grafting may extend the total time of dental implant procedure by several months to grow enough new bone.
Types of bone graft
Your dentist or oral surgeon may use a bone graft to rebuild the jawbone. There are 4 types of bone grafts, include:
- Autograft: the bone graft comes from your own body. The oral surgeon harvests the bone from an intra-oral source such as the chin, or an extra-oral source such as the hip or ribs.
- Allograft: the bone graft comes from humans like autograft. The difference is that the bone is taken from someone else, such as cadaver.
- Xenograft: the bone graft comes from an animal source such as bovine bone.
- Alloplastic grafts: the graft is composed of synthetic material such as calcium phosphate (hydroxyapatite and tricalcium phosphate).
Talk to your dentist or oral surgeon about which type is the best for you.
Minor bone grafting
After the extraction of a tooth, your dentist may perform a minor bone grafting to preserve the bone height and width of the jawbone. The bone graft comes in the form of powder, granules, putty, or gel. First, your dentist will extract the damaged tooth. Then, he/she will place a bone graft granules in the extracted-tooth socket and cover the socket with a collagen membrane. After that, your dentist will close the socket with stitches.
Medium bone grafting
If you have a significant bone loss, your dentist may recommend a medium bone grafting to restore the height and width of the jawbone. First, your dentist will make a small incision in the gum, and place the bone graft granules. Then, he/she will close the incision with stitches.
Major bone grafting
If you have a severe bone loss, your dentist may recommend a major bone grafting. This procedure involves the use of a block of bone from your body (autograft). Your dentist will attach the autograft using screws and plates. Also, your dentist will use a bone graft granules to fill the area and create a smooth jaw-ridge shape. After that, your dentist will cover the graft with a membrane and close the whole area using stitches.
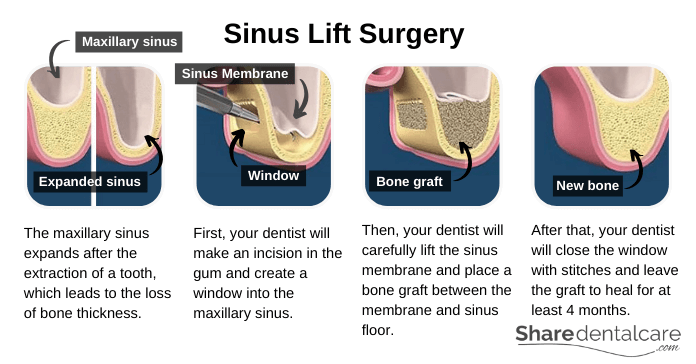
Sinus lift
A sinus lift is a procedure that involves the placement of a bone graft into the maxillary sinus to increase the amount of bone in the upper jaw (premolar and molar teeth area). After the extraction of a maxillary molar or premolar, the bone in this area remodels and loses its height and width. Also, the maxillary sinus expands in this area, which leads to further loss in the bone thickness. So, your dentist may recommend sinus lift to increase the amount of bone and provide support for the dental implant.
First, your dentist will make an incision in the gum and create a window into the maxillary sinus. Then, he/she will carefully lift the sinus membrane and place a bone graft between the membrane and sinus floor. After that, your dentist will close the window with stitches and leave the graft to heal for at least 4 months.
Anesthesia
Since the dental implant procedure is oral surgery, you will need anesthesia to control the pain and make you comfortable during the procedure. Anesthesia options include local anesthesia, sedation, and general anesthesia. The type of anesthesia used depends on:
- The number of dental implants.
- The patient preference.
- The preference of your dentist or oral surgeon.
If you are having one or two implants placed, you will need local anesthesia. General anesthesia is not the best option for the placement of a few implants. Another anesthesia option is conscious sedation, which can be either nitrous oxide or medication. Sedation is used in conjunction with local anesthesia to help you relax during the dental implant procedure. It is beneficial for patients with dental anxiety.
Your dentist or oral surgeon will perform the procedure under general anesthesia if you must have a bone graft (autograft), in which the bone is harvested from your body. In most cases, dentists recommend local anesthesia with or without sedation. Talk to your dentist or oral surgeon about which anesthesia option is the best for you. If you are having conscious sedation or general anesthesia, plan to have a friend or family member take you home after the dental implant procedure.
Dental Implant Procedure (Placement Surgery)
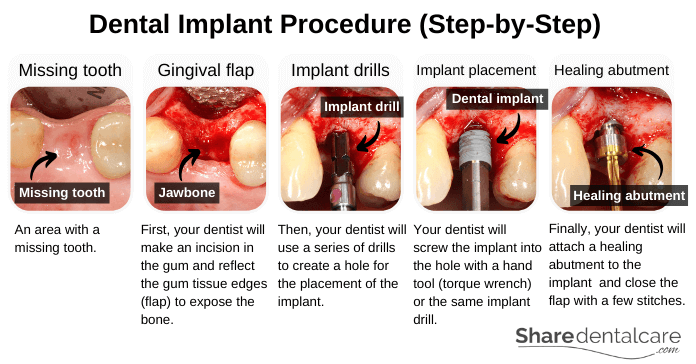
The dental implant surgery is usually performed in the dental office under local anesthesia. The placement of the dental implant involves several steps:
Gingival flap
First, your dentist will make an incision in the gum and reflect the gum tissue edges (flap) to expose the jawbone underneath. There is an alternative technique for the placement of the dental implant, which is known as flapless implant surgery. It is a minimally invasive procedure that is performed using a surgical guide (surgical stent) derived from your CBCT. the flapless implant surgery reduces the surgery time and the post-operative discomfort. However, it will increase the total cost of the dental implant procedure.
Implant drills
After the reflection of gum tissues, your dentist will use a pilot drill to make a small hole in the jawbone (pilot hole). The pilot hole serves as a guide for larger drills used later on. Then, your dentist will expand the pilot hole with larger drills to accommodate the length and diameter of the dental implant. Your dentist will use these drills at a highly regulated speed with cooling saline to keep the temperature low. Overheating can lead to the death of bone cells, causing the failure of the dental implant procedure (failure of osseointegration).
Placement of the dental implant
Your dentist will screw the implant into the hole with either a hand tool (dental torque wrench) or the same implant drill (with a special adapter holds the implant).
Closing the implant site
At this point, your dentist will attach a cover screw or healing abutment to the implant. Then, he/she will reposition the gum tissues back over the jawbone and hold them in place with a few stitches. These stitches are removed after the healing of the gum tissues (seven to ten days). It takes three to six months for the implant to fuse with the jawbone (osseointegration), depending on the quality of bone.
Healing Time (Osseointegration)
After the placement of the implant into the jawbone, the bone begins to grow and fuses with the implant. This process is known as osseointegration, which makes the dental implant permanently stable. The osseointegration can take 3 to 6 months in the upper jaw and 2 to 4 months in the lower jaw, depending on the quality of bone.
Implant movement during the healing period can lead to the formation of fibrous tissue instead of bone, which interferes with the osseointegration and increases the implant failure rates. So, you have to wait until osseointegration is complete before attaching the artificial teeth to the implant. This will minimize the risk of failure. Also, the initial stability of the implant during surgery is an important factor for successful implant osseointegration.
Placing the Abutment
The abutment is the part that connects the implant body to the dental prosthesis such as a crown, bridge, or denture. When osseointegration is complete, your dentist may perform minor surgery under local anesthesia to attach the abutment to the implant body. If the gum covers the implant, your dentist will:
- Make an incision in the gum and expose the dental implant.
- Remove the cover screw that seals the implant.
- Attach the abutment to the implant body.
- Close the gum around the abutment and leave the gum to heal for one to two weeks.
Sometimes, the dentist uses a healing abutment or one-piece implant (the implant body is connected to the abutment) during the dental implant procedure. So, you won’t need a second surgical step because the abutment already appears above the gumline. However, some patients don’t like the appearance of the abutment in their mouth, and it will be visible until the osseointegration is complete. So, they prefer to have the abutment placed in a second procedure (two-stage dental implant procedure).
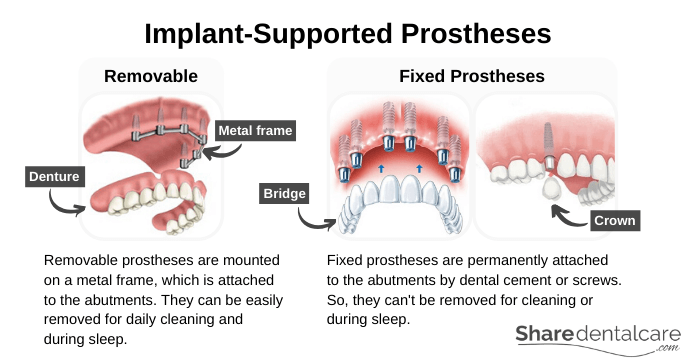
Dental Prosthesis
Placing a dental prosthesis is the final stage of the dental implant procedure. This stage begins once the implant is well integrated, and the abutment is in place. In this stage, your dentist will restore the function and shape of missing teeth. First, your dentist will take a dental impression and send it to the dental lab. The dental technician will use this impression to fabricate a dental prosthesis such as a crown, bridge, or denture. Finally, your dentist will attach this prosthesis to the abutment with dental cement or screws.
Attaching the dental prosthesis to the implant during the osseointegration period can cause implant movement. This movement can lead to the formation of fibrous tissue around the implant instead of bone, preventing the osseointegration and causing implant failure. So, your dentist won’t attach the prosthesis to the implant until osseointegration is complete. Types of the implant-supported prostheses include:
- Removable dental prostheses: for example, partial and complete dentures. They are mounted on a metal frame, which is attached to the implant abutments. You can easily remove the removable prosthesis for daily cleaning and during sleep.
- Fixed dental prostheses: for example, crowns and bridges. They are permanently attached to the implant abutments by dental cement or screws. So, you won’t be able to remove the fixed crown or bridge for cleaning or during sleep. Fixed prostheses are much stronger and more stable than removable prostheses.
What to Expect after the Dental Implant Procedure?
It is normal to experience discomfort after the dental implant procedure. So, your dentist will prescribe painkillers and anti-inflammatory drugs to control the pain. Also, you may experience:
- Gum swelling and bruising.
- Facial swelling and bruising of your skin.
- Minor bleeding.
- Pain at the site of the surgery.
If these signs and symptoms get worse in the day after the surgery, contact your dentist or oral surgeon immediately.
What Is the Success Rate of a Dental Implant Procedure?
The dental implant procedure has a success rate of over 95%. The procedure success is related to:
- The quality and quantity of bone.
- The primary implant stability.
- The condition of the gum.
- Dentist’s skills, qualifications, and experience.
- Patient’s oral hygiene.
- Following the post-operative instructions.
- Medical conditions such as diabetes mellitus.
Post-Operative Instructions
You should follow theses post-operative instructions to speed the healing process and prevent complications.
Bleeding
It is normal to have minimal bleeding after the dental implant procedure during the first 24 hours. So, bite down gently on the gauze for 30-60 minutes after the surgery to stop the bleeding. After 30-60 minutes, remove the gauze and then check the surgical site for bleeding. If bleeding continues, place a new gauze pad for 30 minutes. Repeat as needed. It is normal to see blood in the saliva for 2-3 days following the surgery.
Also, don’t spit, smoke, or touch the implant site with your tongue or finger because these activities will disrupt the clotting process, leading to persistent bleeding.
Swelling
Swelling is a normal body’s response to the dental implant procedure. The swelling usually appears the day after the surgery, maximized over the next 2-3days, and persists for 7-10 days. Immediate use of cold compresses (ice-pack) may minimize the swelling. So, apply the ice-packs continuously to your face over the surgical site (20 minutes on and 20 minutes off) during the first 24 hours. After 48 hours, apply a warm compress (heating pad or warm washcloth) to the swollen area to help resolve the swelling.
Pain
You may experience some pain after the dental implant procedure. It is a normal part of the healing process. So, your dentist will prescribe painkillers such as ibuprofen to control the post-operative pain. The pain will gradually decrease when you take painkillers as prescribed. Make sure that you eat something 15-20 minutes before taking the painkiller to avoid nausea and stomach discomfort.
Diet
Proper nutrition is very important for the healing process. During the first 24 hours after the surgery, you should:
- Eat soft foods such as ice-cream, milkshake, pudding, mashed potatoes, and eggs.
- Avoid foods that may irritate the surgical site such as popcorn, chips, and nuts.
- Avoid hot foods and drinks.
- Don’t drink alcohol.
- Avoid the use of straws to prevent the disruption of the clotting process.
After the first 24 hours, you can gradually return to your normal diet.
Oral Hygiene
After your surgery, you can gently brush your teeth and gums with a soft-bristled toothbrush. However, leave the surgical site undisturbed. During the day following your surgery, rinse your mouth with warm saltwater (½ a teaspoon of salt to a cup of warm water) 2 or 3 times a day. Sometimes, your dentist may prescribe chlorhexidine mouthwash instead of warm saltwater.
Continue rinsing your mouth over the next few days following the surgery and don’t use any mouthwash containing alcohol. Also, don’t smoke for at least 3 days after the surgery because smoking can disturb the healing process.
Activities
Physical activities such as exercise or lifting heavy objects will increase the blood pressure, causing postoperative bleeding and discomfort. So, limit physical activities during the first 48 hours after the surgery. Also, keep your head elevated on a pillow during sleep.
Post-Operative Follow-Up
Your dentist will schedule a follow-up appointment 1-2 weeks after the surgery to check the recovery process. So, go to the appointment on time and contact your dentist if you have questions or problems.
Complications of Dental Implant procedure
The dental implant procedure is highly successful. However, there are possible risks like any surgery.
Complications During the Surgery
- Infection at the implant site: the infection can develop during or after surgery, which can increase the risk of implant failure.
- Nerve injury: the injury can cause numbness or tingling of the lip, tongue, and/or chin.
- Perforation of the maxillary sinus: this can lead to sinus problems and infection in the area.
- Injury to blood vessels: this can lead to excessive bleeding.
- Damage of the neighboring teeth during the surgery.
- Lack of primary implant stability: this increases the risk of implant failure.
Complications in the First 6 Months
- Failure of osseointegration: the implant may fail to integrate with the surrounding bone in the first 6 months due to several factors:
- Poor oral hygiene.
- Heavy smoking.
- High alcohol consumption.
- Infection at the implant site.
- Lack of primary implant stability during the surgery.
- Medical conditions such as uncontrolled diabetes mellitus.
Long-term Complications
- Peri-implantitis: it is an inflammatory process that affects the soft and hard tissues surrounding a dental implant, causing the loss of the bone supporting the implant. Risks factors for developing peri-implantitis include:
- Poor oral hygiene.
- Patients who had previous periodontal disease.
- Smoking.
- Uncontrolled diabetes mellitus.
- Parafunctional habits such as bruxism.
- Fracture of the implant: the fracture can occur in the implant-body, the abutment-screw, or the abutment. If only the abutment fractures, the dentist will replace the abutment and prosthesis. But the fracture of the implant body or abutment screw is a serious complication that can’t be easily treated. The treatment of implant-body or abutment-screws fractures usually consists of the removal of the implant with minimal bone removal, and placement of a new dental implant. But the remaining bone may not be sufficient to support the new implant.
- Aesthetic problems: gum recession can lead to the exposure of the metal abutment that holds the prosthesis. Bone loss can lead to the appearance of black triangles between implants and natural teeth.
Conclusion
Do you have a missing tooth/teeth? Dental implants are the best treatment option to replace a missing tooth/teeth. However, they are not suitable for everyone. So, you will need to schedule an appointment with your dentist for an initial consultation. During this appointment, your dentist will examine your mouth, take an x-ray, and ask you about your medical history. Also, your dentist will ask for a cone-beam computed tomography (CBCT) to evaluate the height, width, and density of the jawbone. If you are a good candidate for dental implants, your dentist will talk with you about the steps of the procedure.
The dental implant procedure is accomplished in 2 stages. In the first stage, the dentist places the implant body in the jawbone and leaves it to heal (osseointegration) for 4 to 6 months, depending on the quality of bone. In the second stage, the dentist attaches the abutment to the implant body and then places the dental prosthesis (crown, bridge, or denture). The entire procedure can take 6 to 8 months. It may take longer if bone grafting is needed. The dental implant procedure is highly successful, with a success rate of over 95%.