People with diabetes are at an increased risk for developing oral health problems, such as gum disease and tooth decay. So, If you have diabetes, it’s important to take steps to keep your teeth and gums healthy. In this blog post, we will discuss how diabetes can affect your teeth and what you can do to protect your oral health.
What is Diabetes & Does It Affects Your Teeth?
Diabetes is a chronic health condition that causes high blood sugar levels. It can happen when the pancreas does not produce enough insulin (a hormone that regulates blood sugar levels) or when the body does not properly use the insulin it produces (insulin resistance).
Poorly controlled diabetes can lead to several health complications, including heart disease, kidney disease, eye damage, and nerve damage. Also, uncontrolled diabetes can negatively affect your teeth and oral health. People with diabetes are at an increased risk of developing gum disease and tooth decay.
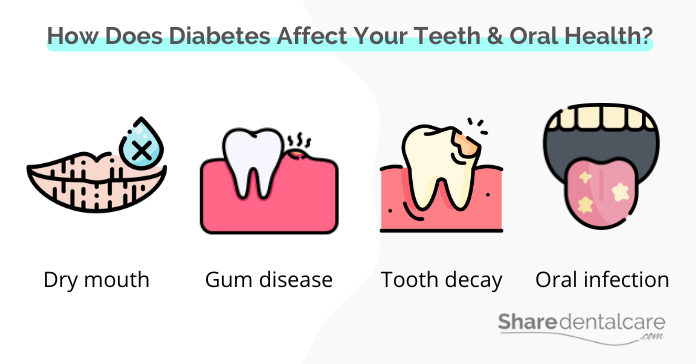
How Does Diabetes Affect Your Teeth & Oral Health?
Diabetes can affect the health of your teeth and gums in a few different ways, including:
- Dry mouth: Diabetes can reduce the production of saliva, leading to a condition called xerostomia, or dry mouth. Saliva is important for keeping the mouth moist and washing away food and bacteria. Dry mouth condition increases the risk of gum disease and tooth decay.
- Gum disease: Diabetes weakens the body’s ability to fight infection, which can lead to an increased risk for gum disease. Gum disease is a bacterial infection of the gums that can cause redness, swelling, and bleeding. If left untreated, gum disease can lead to tooth loss.
- Tooth decay: The high sugar levels in saliva associated with diabetes provide the perfect environment for bacteria to grow. These bacteria decompose sugars and produce acids, which can damage teeth and lead to tooth decay. Besides, a dry mouth can also increase the risk of tooth decay. You can read more about the link between diabetes and teeth breaking.
- Poor healing: Uncontrolled diabetes can also delay the healing process. This is a problem with dental procedures that require surgery, such as tooth extraction and dental implants.
- Oral infection: Diabetes can also increase the risk of developing fungal infections of the mouth, such as thrush. Thrush is an infection caused by the Candida albicans fungus. It can cause white, patchy lesions on the tongue and inside of the cheeks.
Uncontrolled diabetes can negatively affect your teeth and cause serious oral health problems. So, it’s important to take steps to protect your teeth and gums if you have diabetes.
When To See A Dentist?
Some oral health problems, such as gum disease and tooth decay, can be difficult to spot in the early stages. That’s why it’s important to see your dentist regularly, even if you don’t have any obvious oral health problems. There are a few signs and symptoms to look out for that may indicate that diabetes is negatively affecting your teeth and gums, including:
- Red, swollen, or bleeding gums
- Gums are tender to touch
- Dry mouth
- Receding gums
- Bad breath that doesn’t go away with brushing and flossing
- Loose teeth
- Change in the way your teeth fit together when you bite
- Spaces developing between your teeth
- Slow healing after dental procedures
If you have any of these signs or symptoms, see your dentist as soon as possible. They can determine if you have a dental or oral health problem and develop a treatment plan to treat it.
Preventing Teeth Problems When You Have Diabetes
People with diabetes are prone to conditions that may negatively affect their teeth and oral health. Good oral care is important for people with diabetes to help prevent these problems.
Here are some tips for preventing teeth problems when you have diabetes:
- Control your blood sugar levels: Keep your blood sugar levels under control to help reduce your risk for oral health problems.
- Practice good oral hygiene: This means brushing your teeth at least twice a day with fluoride toothpaste, flossing daily, and using mouthwash.
- Quit smoking: Smoking can increase the risk of gum disease and tooth decay. People with diabetes who smoke are more likely to develop oral health problems than those who don’t smoke.
- Eat a healthy diet: A healthy diet is important for overall health, including oral health. Be sure to eat plenty of fruits, vegetables, and whole grains. Avoid sugary foods and drinks.
- Drink plenty of water: Drinking water helps keep your mouth moist and washes away food and bacteria.
- Visit your dentist regularly: Visit your dentist every 6 to 12 months for a professional cleaning and checkup.
Conclusion
Diabetes can affect your teeth and oral health in many ways. Diabetes decreases saliva production, which increases the risk of gum disease and tooth decay. Also, the high sugar levels in saliva associated with diabetes provide the perfect environment for bacteria to grow. It’s important to practice good oral hygiene and control your blood sugar levels to help prevent these problems. Be sure to visit your dentist regularly for a professional cleaning and checkup.