Gum pockets are spaces between the tooth and gum that form when the gums pull away from teeth due to periodontal disease. These gum pockets increase in depth and become infected if left untreated. In the early stage, the infected gum pocket can be treated with good oral hygiene and professional teeth cleaning. Over time, the infection can damage the bone and tissues that support teeth and may eventually lead to tooth loss. In this blog post, we will discuss how does a gum pocket forms, how it becomes infected, and how to prevent it from developing.
How Does an Infected Gum Pocket Form?
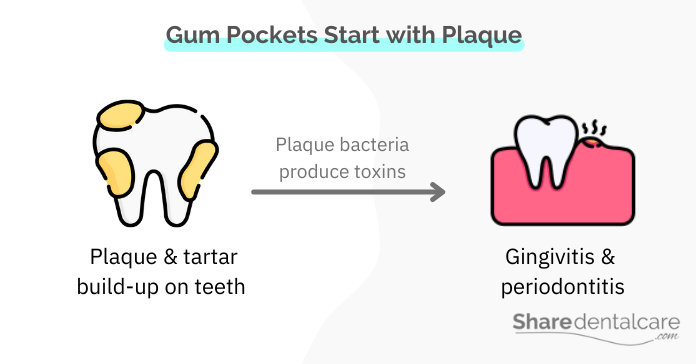
When you don’t brush your teeth regularly, plaque and bacteria will build up on your teeth and gums. Dental plaque is a sticky film that forms on the teeth and is composed of bacteria, food debris, and saliva. If not removed by brushing or flossing, the plaque will harden into tartar, which is a yellowish-brown mineral deposit that can only be removed by a dental professional.
The bacteria in plaque and tartar produce acids that irritate the gums, causing periodontal disease (gum disease), which can be categorized into:
- Gingivitis: gingivitis infection is an early stage of periodontal disease that causes the gums to become red, swollen, and bleed easily.
- Periodontitis: it is a more advanced stage of periodontal disease that can damage the bone and tissues that support teeth, leading to tooth loss.
Gingivitis causes the gums to become red, inflamed, and swollen. Eventually, the gums separate from the teeth as a response to the inflammation and form a pocket. As periodontal disease progresses, the pocket deepens, and more plaque and bacteria accumulate below the gum line, which makes the gum pocket infected. Over time, the infection will damage the bone and tissues that support teeth, leading to tooth loss.
Risk Factors for Infected Gum Pocket
Some factors can increase the risk of periodontal disease and infected gum pocket, including:
- Poor oral hygiene habits.
- Smoking or chewing tobacco. Read more about how you get gum disease from tobacco.
- Crooked teeth, which are harder to clean.
- Hormonal changes during pregnancy, puberty, and menopause.
- Vitamin C deficiency
- Certain medications, which cause dry mouth.
- Some diseases such as diabetes, AIDS, and leukemia.
- Medical conditions that affect the immune system, such as leukemia, HIV/AIDS, and cancer treatment
- Certain diseases, for example, diabetes, rheumatoid arthritis, and Crohn’s disease.
The Depth & Severity of Gum Pockets
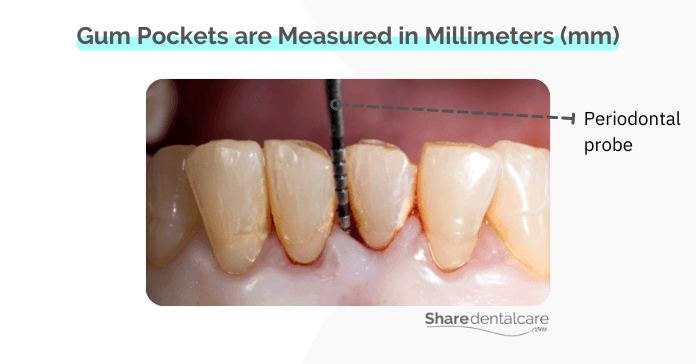
In a healthy mouth, the gums fit snugly against the teeth, and there are no spaces between them. The gum pocket process begins with gingivitis and becomes deep and infected if left untreated. The greater the gum infection, the greater the depth of the pocket. Some pockets are shallow and barely noticeable, while others can be deep and cause discomfort and pain.
The severity of a gum pocket is determined by its depth, which is measured in millimeters (mm). The dentist uses a periodontal probe to measure the depth of the pocket.
- Healthy pocket: 3mm or less in-depth
- Mild pocket: 3-4mm in-depth
- Moderate pocket: 5-7mm in-depth
- Severe pocket: 7-12mm in-depth
Dentists use gum pocket measurements to determine the severity of periodontal disease and infection. The greater the pocket depth, the greater the level of infection and inflammation, the greater the destruction of the bone and tissues that support teeth.
When to See a Dentist?
The early stage of periodontal disease doesn’t usually cause pain, so many people ignore it until it becomes more serious. It’s important to see a dentist if you notice any of the following signs and symptoms of periodontal disease:
- Red, swollen gums.
- Gum bleeding when brushing and flossing.
- Persistent bad breath that doesn’t go away.
- Gum recession, which makes the root of the tooth more visible.
- Painful chewing.
- Development of gum pockets between teeth.
- Pus between the gum and tooth.
- Loose teeth or teeth that are shifting position
How Infected Gum Pocket is Treated?
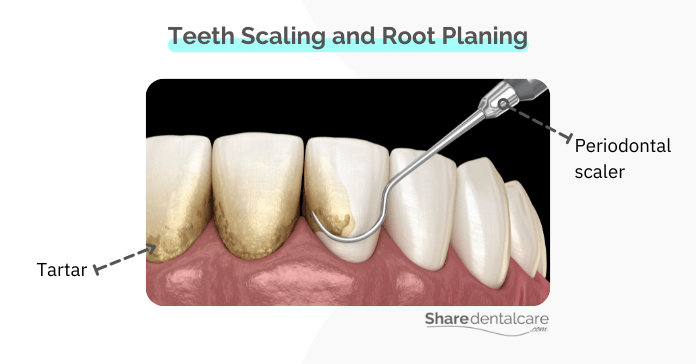
The treatment depends on the depth of the pocket and how far periodontal disease has progressed. Small to moderate gum pockets are usually treated with non-surgical treatment such as scaling & root planing, while severely infected pockets may need surgery.
Non-Surgical Treatment
- Improving oral hygine: small pockets can be reduced and treated by improving oral hygiene habits and scaling, which is performed using periodontal instruments, a laser or an ultrasonic device.
- Scaling and root planing: if the pockets are deeper, your dentist may recommend a scaling and root planing procedure to remove the plaque and tartar (calculus) from below the gum line. The dentist will also smooth the root of the tooth to help make the area less likely to harbor bacteria in the future.
- Antibiotics: your dentist may prescribe antibiotics to help control the infection.
Read more about how to reduce gum pockets naturally.
Surgical Treatment for Infected Gum Pocket
If the gum pocket is too deep or severely infected, your dentist may recommend surgical treatment. Surgical procedures are usually associated with scaling and root planing, and antibiotic treatment to help control the infection.
- Flap surgery (pocket reduction surgery): your dentist may raise a flap for effective scaling and root planing. The gum tissue will then be sutured back in place. This surgery is designed to reduce the depth of the pocket.
- Bone graft: if too much bone has been lost, a bone graft may be needed to replace it. The bone graft comes from another part of your body, a donor, or synthetic material. Read more about reversing periodontal disease bone loss.
- Soft tissue graft: this surgery is used to replace the damaged gums with healthy gum tissue from another part of your mouth.
- Tooth Extraction: if there is severe bone loss and tooth mobility, your dentist may recommend extraction of the affected tooth and replacing it with a dental implant or bridge.
Home Care for Prevention
- Good oral hygiene habits are essential for the prevention of infected gum pockets, including:
- Brush at least twice a day for two minutes.
- Floss daily to help remove food particles and plaque from between teeth, which are hard to reach with a toothbrush.
- Use an antimicrobial mouthwash to help control the growth of bacteria.
- Quit smoking or at least smoke in moderation. Read more about how gums heal after quitting smoking.
- Visit your dentist every six months for checkups and professional teeth cleanings.
Infected Gum Pocket – Conclusion
A gum pocket is a space between the tooth and gum that forms as a result of periodontal disease, an infection of the gums. As the periodontal disease progress, the gum pockets become deeper and infected, causing pain. The treatment of the gum pocket depends on its depth, which is determined by a dental examination.
For small to moderate pockets, the treatment is non-surgical, which means improving oral hygiene habits and professional teeth cleaning. For deeper or severely infected pockets, surgery may be required. If you noticed any signs or symptoms of periodontal disease, it is important to see your dentist as soon as possible to prevent complications. Good oral hygiene habits are essential for the prevention of infected gum pockets.