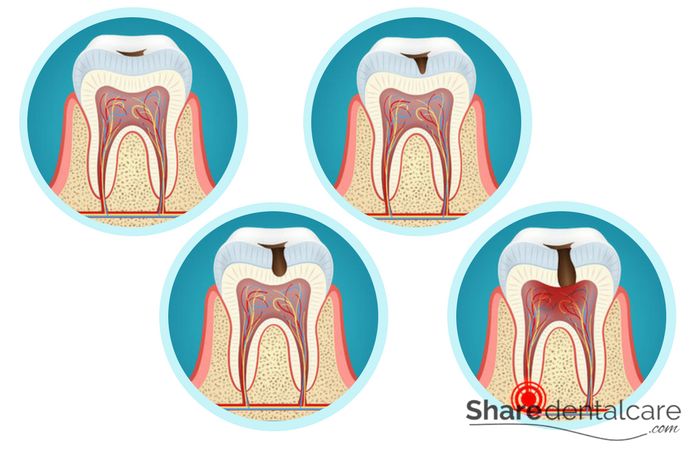
Dental caries, also known as tooth decay, is the destruction of teeth caused by bacteria in the mouth. These bacteria accumulate on teeth surfaces and produce acids that damage the tooth enamel. In the early stages, dental caries appear as pale or brownish spots on teeth. Then, it turns later to dark brown or black spots. If left untreated, caries will extend into the dentin (the second layer in the tooth) and eventually infect the tooth pulp. In the late stages, dental caries can lead to a dental abscess or tooth loss.
Prevalence of Dental Caries
Dental caries (tooth decay) is one of the most common diseases in the world and occurs with a high incidence in industrialized countries. In the early phases of human history, it is hardly noticed. A change in the diet of industrially advanced countries in the 19th century led to a sharp increase in dental caries rate. Almost everyone is affected once in his life by caries. The finer the food preparation and a lower proportion of hard food components ensure that the occlusal surfaces and notches in the tooth surface (pits and fissures) are susceptible to tooth decay. Also, it affects the cervical region and between teeth. Today, caries occurs more in the child’s primary teeth and tooth roots in older people.
The Process of Dental Caries Formation
Dental caries bacteria decompose sugar from food debris and produce acidic metabolites (mainly lactic acid), which destroy the tooth enamel. The tooth enamel is exposed constantly to two processes:
- Demineralization: Bacteria decompose sugar and produce acids in the oral cavity which decrease the oral pH and create an acidic environment. In response calcium and phosphate ions diffuse out of the tooth enamel, resulting in demineralization. The pH is a measure of the acidic or basic character of an aqueous solution. Solutions with a pH less than 7 are acidic and solutions with a pH greater than 7 are basic.
- Remineralization: When the pH rises again, the tooth enamel restores calcium and phosphate from saliva (The process is reversed).
Dental caries is a dynamic process characterized by episodic demineralization and remineralization. Any alteration in the balance of these dynamic processes can cause caries, which leads to tooth enamel damage.
Signs and Symptoms of Dental Caries
Dental caries symptoms depend on the stage. In the early stages, caries may cause superficial changes in tooth enamel. In the late stage, a visible cavity may form on the tooth surface.
Early Stage Symptoms
Dental caries at the early stages are barely visible. You may find white spots on the tooth surface. These white spots are solved minerals from tooth enamel. The Early stage of caries can be reversed by regular tooth brushing to remove caries bacteria and by using fluoride toothpaste to replace mineral loss from the tooth surface.
With poor oral hygiene, the progression of caries begins. White spots on the tooth enamel turn to cavities, and you may experience pain for the first time. But pain occurs when the nerves of the tooth are attacked by bacteria. At the early stages of dental caries, teeth may react very sensitively to cold or high-sugar foods.
Late Stage Symptoms
Untreated caries progress slowly to the pulp, and the pain may increase. You may notice a hole in the tooth (cavity). Late-stage caries can cause a dental abscess or even tooth loss.
Secondary Caries
Dental caries treatment (tooth filling or dental crowns) does not guarantee that you are protected from caries. With poor oral hygiene, teeth often develop so-called secondary caries. It is formed over several years at the interface between the tooth and the filling or crown. This too-small area is large enough to allow the microscopic bacteria to grow. Secondary caries may be the reason for loose or lost tooth fillings, a lasting or recurrent toothache, and tooth sensitivity with sweet, hot, or cold foods and drinks. However, these symptoms occur in the late stage of dental caries.
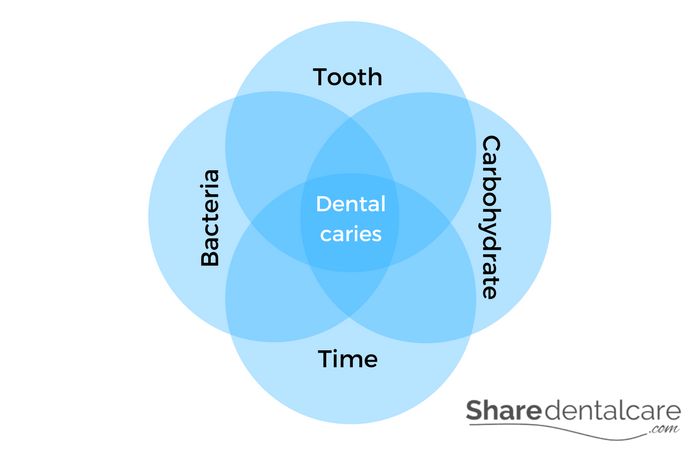
Causes of Dental Caries
Dental caries are a multifactorial process that is caused by several factors, including:
- Poor oral hygiene: Lack of dental care promotes bacterial growth, proliferation, and the formation of plaque, a sticky, colorless film of bacteria that forms on teeth.
- Bacteria: They decompose carbohydrates and produce acidic metabolites that attack tooth enamel.
- Carbohydrate: it provides the basis of life for bacteria.
When sugary food sticks or accumulates on the tooth surface. Oral bacteria decompose sugar and produce acidic metabolites that attack the tooth enamel and promote the development of caries. Dental caries are not hereditary. However, it can occur frequently in families whose members have a “caries-prone” tooth form, for example, deep tooth fissure. Also, oral hygiene and bad eating habits can lead to a frequent occurrence of caries within a family.
Saliva
The amount and composition of saliva influence the spread of caries. Saliva softens the food, so it makes the removal of food debris easier. The saliva:
- Neutralizes the acid produced by bacteria.
- Decreases plaque accumulation.
- Aids in the removal of food debris.
- Promotes remineralization by acting as a reservoir of calcium, phosphate, and fluoride ions.
- Has antibacterial action.
If you can’t brush your teeth after eating. You can chew sugar-free gum with sugar substitute xylitol. Chewing sugar-free gum stimulates saliva production and may partially neutralize the acid produced by bacteria.
Risk Factors for Dental Caries
Dental caries are influenced by several factors; bacteria, oral hygiene, and eating habits. In the mouth, there are more than 700 types of bacteria. These microorganisms are needed for healthy oral flora. Some bacteria feed on sugar and produce acidic metabolites. These acids attack the tooth enamel, causing caries. The following factors increase the risk of dental caries:
- Poor oral hygiene: irregular toothbrushing and flossing, especially after eating and drinking will lead to plaque accumulation on tooth surfaces, gumline, and in interdental spaces.
- Dry mouth: saliva protects your teeth against dental caries by washing away bacteria and food debris. Saliva has an antibacterial effect and buffering effect that reduce the level of acids produced by oral bacteria. Also, it contains minerals (calcium, phosphate, and fluoride ions) that can reverse early-stage caries (Remineralization). The low salivary flow will increase the risk of dental caries.
- Some foods and drinks: dental caries formation is promoted by sugary foods and drinks. Carbohydrates provide a good environment for bacterial growth. Oral bacteria decompose sugar and produce acidic metabolites that damage the tooth enamel.
- Smoking: smoking or chewing tobacco promotes dry mouth condition (xerostomia), causing tooth decay.
- Some diseases: anorexia, bulimia, heartburn, or gastroesophageal reflux disease, can cause acid to flow into the oral cavity causing tooth erosion and dental caries.
Complications of Dental Caries
In the early stage, dental caries (tooth decay) affects only tooth enamel. Untreated caries create a cavity in the tooth enamel, which can spread to the dentin (the second layer of the tooth after enamel) and eventually reach the tooth pulp (which contains nerves and blood supply). It can cause serious and lasting complications, such as:
- Severe pain.
- A dental abscess.
- Tooth fracture.
- Eating problems.
- Tooth loss.
Also, tooth decay bacteria can:
- Enter the bloodstream, causing blood poisoning (sepsis).
- Spread to the soft tissue, causing facial cellulitis and Ludwig’s angina.
- Spread to the bone of the jaw, causing osteomyelitis.
- Reach the heart via the bloodstream, causing endocarditis.
How Dental Caries are Diagnosed?
Your dentist will examine your oral cavity with a mirror, probe, and x-ray, searching for evidence of caries. It is often very difficult to detect caries in the early stage. Your dentist may detect cavities in the tooth enamel extending to the pulp in the late stage. Treatment options depend on the diagnosis (the position and extension of tooth decay). Dental caries is not hereditary but occurs frequently in a family. This is probably due to similar eating and oral hygiene habits in the family.
Treatment Options for Dental Caries
The treatment depends on dental caries (tooth decay) position and extension. the dentist has various ways to remove it and restore the tooth’s shape and function.
Early Stage Treatment
In the early stage of caries, there are white spots and no cavities on tooth surfaces. In this stage, dental caries can be reversed. For that, you should improve your oral hygiene and change your eating habits. People who consume large amounts of sugary foods and drinks (such as sweets, soft drinks, and juices) have an increased risk that dental caries will continue to spread and cavities will occur on tooth surfaces.
So, brush your teeth regularly with fluoride toothpaste to promote remineralization. And chew sugar-free gum to stimulate the salivary flow that flushes out bacteria and food debris and neutralizes acids produced by oral bacteria. Also, you should visit your dentist for professional cleaning and the removal of dental plaque. In the early stage of caries, regular professional fluoridation is recommended to reverse tooth decay through remineralization. The dentist will remove the dental plaque and calculus and will apply fluoride varnish to the affected areas.
Late Stage Treatment
Late-stage caries treatment depends on where and how far it has already progressed. In most cases, the dental drill is used to remove bacteria from cavities. The treatment is performed under local anesthesia.
- Dental fillings, such as amalgam, composite resin, and ceramics. The dentist will remove dental caries by the drill under local anesthesia. To remove bacteria and prevent its progress. Dental fillings are used to restore tooth shape and function.
- Root canal treatment: If dental caries bacteria reached the tooth pulp, you will need a root canal treatment to remove bacteria from the roots and to prevent a dental abscess. Root canal treatment is used to save a badly damaged tooth and prevent its extraction.
- Dental crown: If the tooth becomes weak, you will need a dental crown. It is recommended in a tooth with large restoration and after root canal treatment to protect the tooth and restore its shape and function.
- Tooth extraction: If the tooth is severely damaged and can’t be restored with dental fillings or dental crowns, it must be extracted.
How to Prevent Dental Caries?
You can prevent dental caries by following a few habits every day, mainly oral hygiene and eating habits. Complete removal of dental plaque by regular teeth cleaning is the most effective way to get healthy teeth and gums.
- Regular tooth brushing: at least twice a day, following the correct brushing technique.
- Dental floss: use dental floss and interdental brushes to remove plaque in the interdental spaces and along the gumline.
- Fluoride: gel, toothpaste, and mouthwash with fluoride make your teeth stronger and more resistant to caries. Visit your dentist to know, what is the appropriate amount of fluoride for you.
- Healthy diet: eat a varied diet with plenty of vegetables and fruits, to clean your teeth naturally.
- Reduce the consumption of sugary foods and drinks: foods and drinks that contain a large amount of sugar are bacteria’s food source. Bacteria decompose sugar and produce acidic metabolites that attack the tooth enamel, causing tooth decay.
- Drink plenty of water: to keep your oral cavity moist, wash your teeth from bacteria and food debris, and neutralize bacterial acids.
- Chew sugar-free gum: to stimulate the flow of saliva and inhibit dental caries bacteria.
- Visit your dentist: at least twice a year for professional cleaning and examination. The sooner caries are detected, the better the prognosis.