Molars are large, strong teeth at the back of the mouth. They have a large surface area, which helps grind food before swallowing and digestion. Adults usually have 12 molars (6 molars per arch). Like any tooth, cavities in molars may occur. The risk of cavities is higher in molars than front teeth because molars have pits and grooves. Dental plaque and food particles get stuck easily in these grooves for a long time.
If you don’t clean your teeth well, certain bacteria in the mouth will convert food into acid, which breaks down the tooth enamel. In the early stage, dental caries appears as white spots on molars. As caries advance, holes begin to form, which are known as cavities. Over time, cavities gradually become bigger and may extend to deeper layers, causing pain and dental abscess.
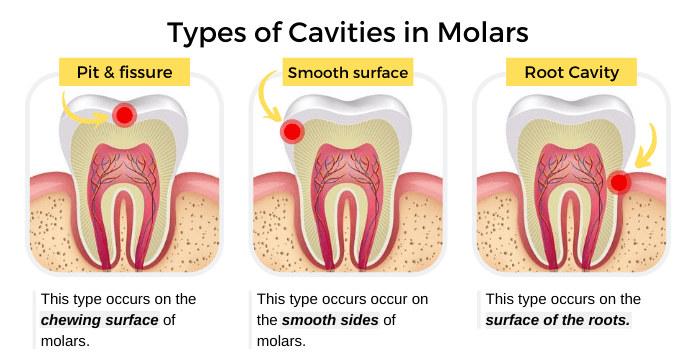
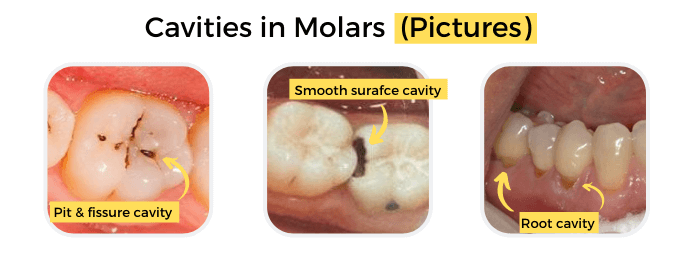
Types of Cavities in Molars
Cavities are caries areas that progress into holes or tiny openings. Types of cavities in molars are:
- Pit and fissure cavities: this type occurs in the chewing surface (occlusal) of teeth. Because the chewing surface of molars contains grooves. The plaque and food particles get stuck easily in these grooves for a long time, increasing the risk of cavities.
- Smooth surface cavities: this type occurs on the exterior flat surface of the teeth. For example, interproximal cavities, which occur on the smooth surface between teeth.
- Root cavities: this type is common in older adults because of the gum recession and the exposure of root surfaces. When gum recession occurs, the root surfaces become exposed and become susceptible to bacteria and cavities.
Symptoms of Cavities in Molars
The signs and symptoms vary, depending on the extent of cavities and proximity to the tooth pulp. In the early stage, you may not have any symptoms at all. As caries advance, cavities in molars become larger. They may cause these signs and symptoms:
- In the early stage, dental caries appears as white spots or lines on teeth surfaces.
- Cavities in molars appear as brown or black holes.
- Toothache.
- Tooth sensitivity to sweet, hot, and cold.
- Pain associated with chewing.
- Gum swelling.
- Pus discharge and bad taste.
- Facial swelling.
Causes of Cavities in Molars
Cavities in molars are permanent damage that appears as brown or black holes. Dental plaque is a sticky colorless film that forms on molars surfaces. This occurs due to eating a lot of sugars and starches, and not cleaning your teeth well. Bacteria in the mouth feed on the sugars in plaque and produce acid. This acid dissolves the tooth enamel (demineralization), which can lead to the formation of holes or tiny openings in the enamel surface. As cavities in molars advance, the bacteria may reach the second layer in molars (dentin). Also, they continue their progress and can reach the tooth pulp, which contains nerves and blood vessels.
Risk Factors
Several factors increase the risk of cavities in molars, including:
- Tooth location: cavities occur most often in molars and premolars because they have lots of grooves and pits. These grooves collect food particles and are harder to keep clean than smoother front teeth.
- Inadequate tooth brushing and flossing: if you don’t clean your teeth well after eating or drinking, plaque will form quickly on molars surfaces.
- Eating carbs and sugary foods: caries bacteria feed on carbs and sugary foods, producing acids that destroy the teeth.
- Older age: older adults are at higher risk for root cavities. When gums recede, the roots become exposed, and root cavities can occur.
- Not getting enough fluoride: fluoride makes the enamel more resistant to caries and helps prevent cavities. Also, the early stage of dental caries can be reversed by fluoride (remineralization).
- Dry mouth: saliva wash away plaque and food. Also, it helps counter the bacterial acid. The lack of saliva increases the risk of cavities in molars. Dry mouth can occur due to medical conditions, medications, or mouth breathing.
- Braces and broken tooth fillings: they allow the build-up of plaque more easily and make it harder to clean.
- Eating disorders: in bulimia, stomach acid in vomit dissolve the tooth enamel and lead to cavities in molars.
Diagnosis
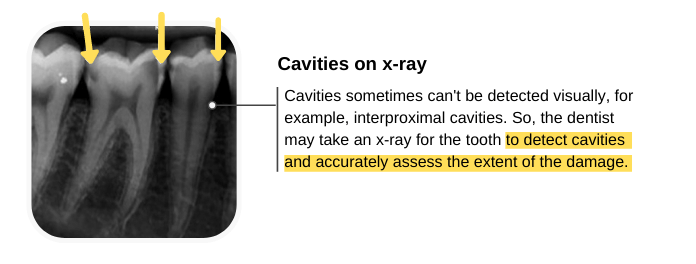
You may not be aware that you have cavities in molars because they are usually not visible. That is why it is important to visit your dentist regularly for a dental check-up and professional cleaning. Your dentist will examine your mouth to detect any problems such as gum disease, cavities in molars. Methods of diagnosis include:
- Oral examination: your dentist will examine your mouth with dental instruments (mirror and probe). With these instruments, the dentist can detect cavities in places that are not visible to you.
- X-ray: cavities sometimes can’t be detected visually, for example, interproximal cavities. So, the dentist may take an x-ray image for the molars to determine the location and extent of the damage. Types of x-rays used: bite-wing, periapical, and panoramic x-ray.
Cavities in Children
Dental caries and cavities are a common problem in children. This problem occurs due to the accumulation of plaque on teeth surfaces and not cleaning the child’s teeth regularly. Bacteria in plaque feed on carbohydrates and turn them into acid. This acid attacks the tooth enamel and may lead to the formation of cavities. Every child is at risk for cavities in molars, but some children have a higher risk. Risk factors include:
- Consumption of too many sugary and acidic foods and drinks.
- Poor oral hygiene (not cleaning your child’s teeth regularly).
- Not getting enough fluoride.
- Bedtime infant feeding. Giving your baby a bedtime bottle filled with milk, formula, or juice increases the risk of cavities in baby teeth.
- Dry mouth.
Cavities in molars occur more often than in front teeth because molars have grooves that can trap food particles.
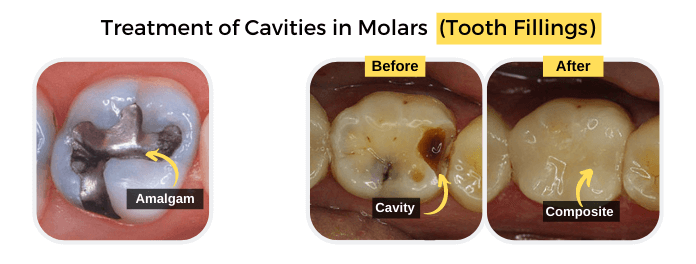
Treatment of Cavities in Molars
The treatment of cavities in molars vary, depending on the size and extent of the cavities. The treatment includes:
- Tooth fillings: under local anesthesia, the dentist will remove cavities in molars with a dental drill. Then, they will place tooth fillings to restore the shape and function of teeth. Types of tooth filling include amalgam, composite, and glass ionomer.
- Root canal treatment: when bacteria reach the tooth pulp, this will cause pain and inflammation of the pulp tissues. So, your dentist may recommend a root canal treatment.
- Pulpotomy/pulpectomy: when cavities in baby teeth reach the pulp, your child’s dentist may recommend pulpotomy or pulpectomy. A pulpotomy is the partial removal of the baby tooth pulp, while pulpectomy is the complete removal of the pulp.
- Dental crowns: if the molar is damaged and can’t be restored by tooth fillings, you may need a dental crown. Dentists usually recommend dental crowns after root canal treatment.
- Tooth extraction: if the molar is severely damaged and can’t be restored by tooth fillings or crowns, the dentist often recommends the removal of the tooth.
Prevention of Cavities in Molars
To prevent cavities in molars, you should:
- Brush and floss your teeth regularly: you should remove the dental plaque regularly from teeth surfaces by using a soft-bristled toothbrush. Also, use dental floss to remove the plaque that accumulates between teeth.
- Use fluoride toothpaste: fluoride helps in the prevention of cavities in molars. Also, it helps reverse the early stage of dental caries.
- Rinse your mouth: your dentist may recommend the use of a mouthwash with fluoride to help prevent cavities.
- Fissure sealants: a sealant is a protective plastic coating, which is applied to the chewing surface of molars. It seals the grooves and prevents food and bacteria from getting into these grooves.
- Eating healthy foods: fruit and vegetables increase saliva flow, which washes away food particles and counter bacterial acids. Also, avoid sugary foods and drinks because they increase the risk of cavities in molars, for example, cake, candies, cookies, soda, and fruit juice.
- Fluoride treatment: you may need a periodic fluoride treatment if your risk of cavities is very high.
- Visit your dentist regularly: Visit your dentist at least once every 6 months for professional teeth cleaning and regular check-up. Your dentist can spot problems early.
Summary
- Molars are large, strong teeth at the back of the mouth.
- They help grind food before swallowing and digestion.
- Cavities most often occur in posterior teeth (premolars and molars) because they have a lot of grooves and pits that can collect food particles.
- Certain bacteria in the mouth convert food into acid that breaks down the tooth enamel.
- Cavities usually appear as holes or tiny openings in molars.
- Types of cavities in molars are pit & fissure, smooth surface, and root cavities.
- Cavities are a common problem in children.
- The treatment includes tooth fillings, root canal treatment, or tooth extraction, depending on the extent of the damage.
- Brush your teeth regularly with fluoride toothpaste. Also, visit your dentist at least once every 6 months for professional cleaning.